Soap notes mental health examples
Home » Doctor Visit » Soap notes mental health examplesSoap notes mental health examples
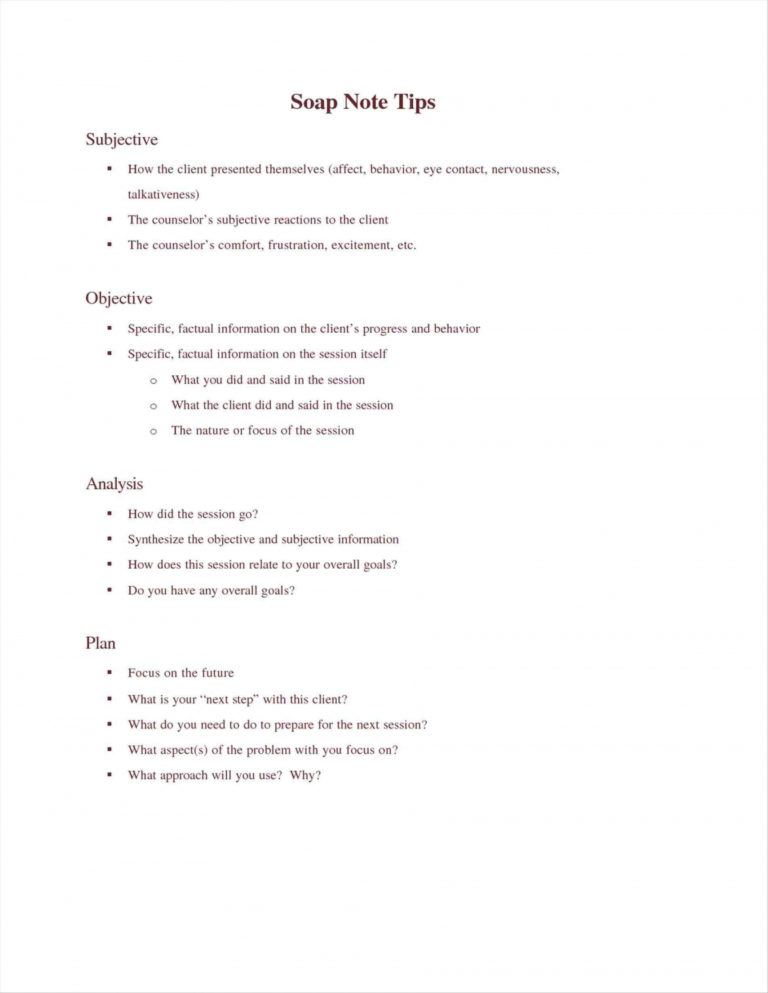
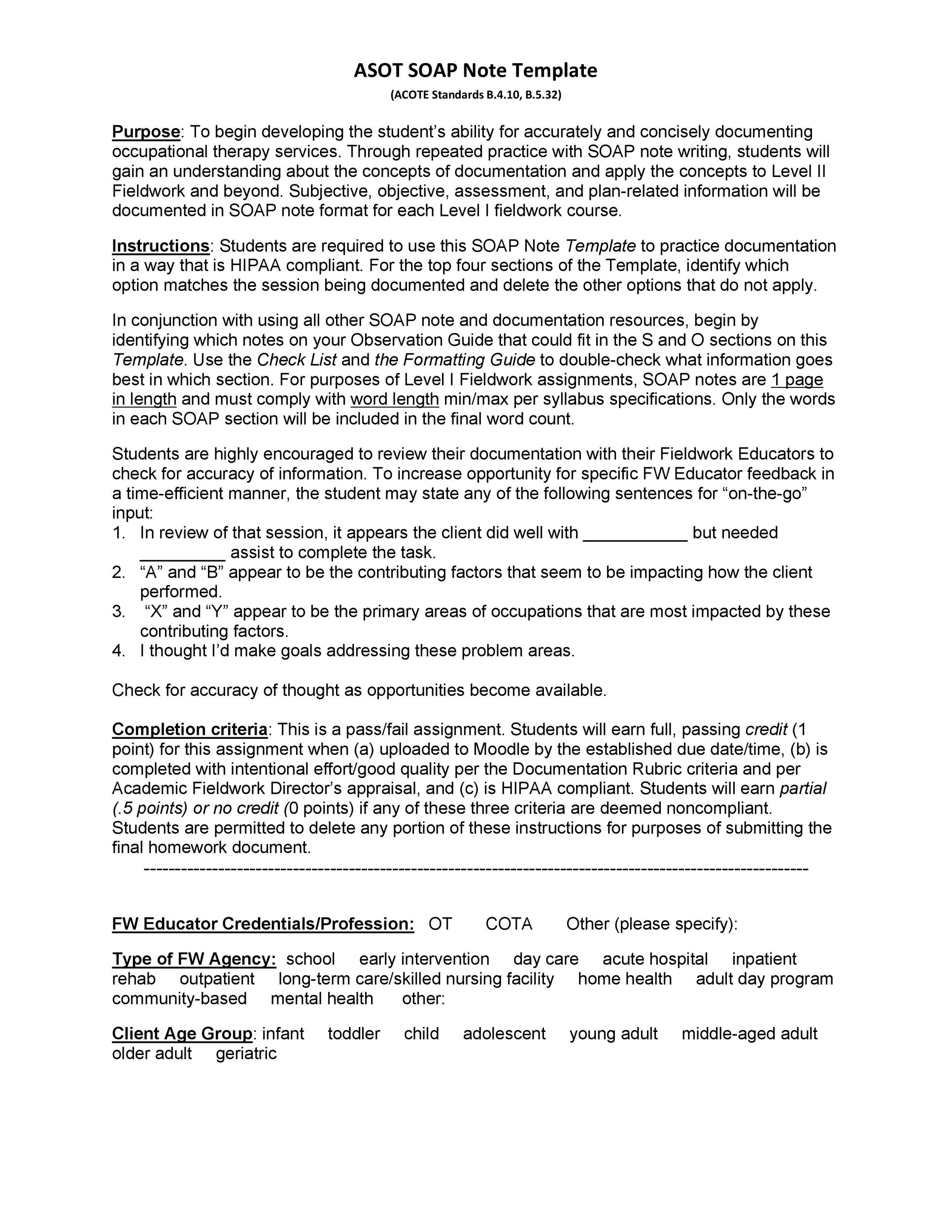
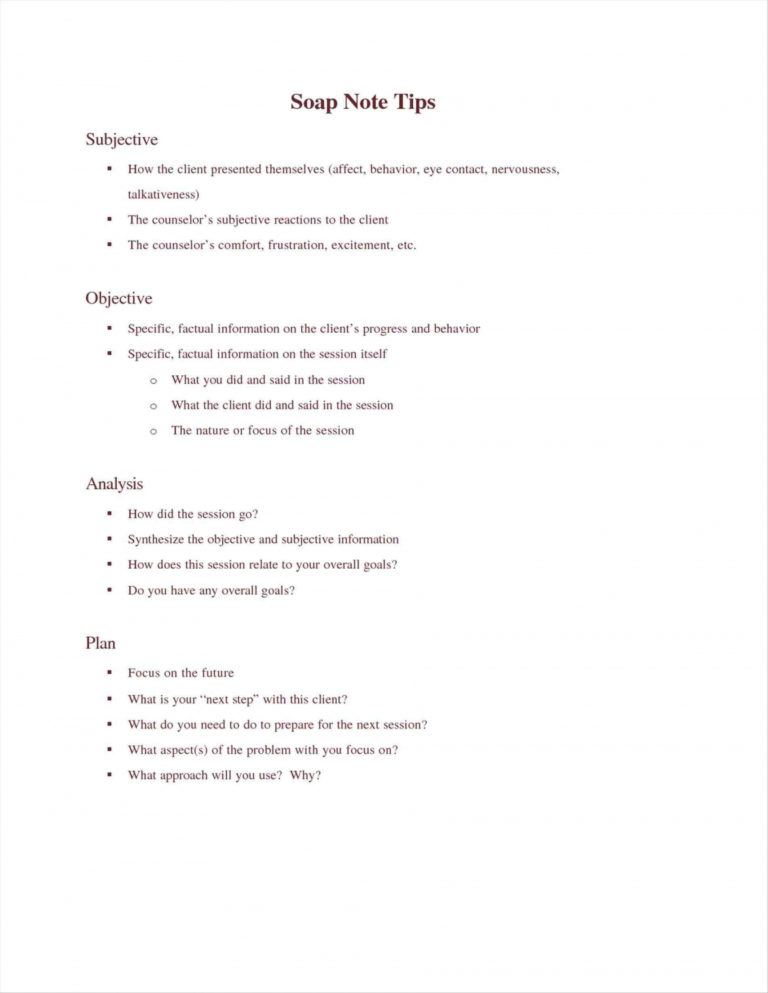
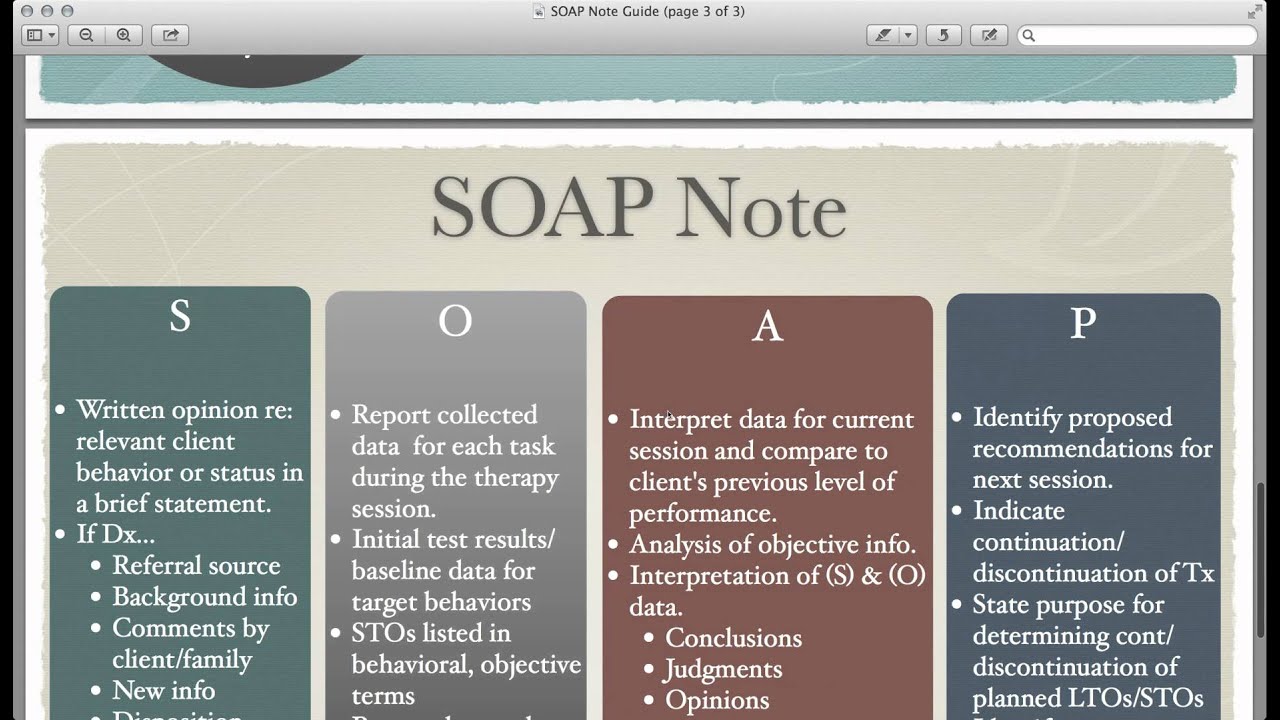
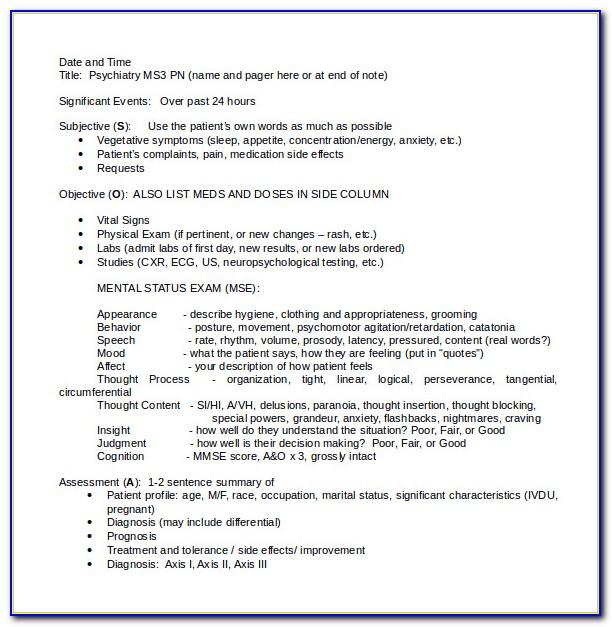
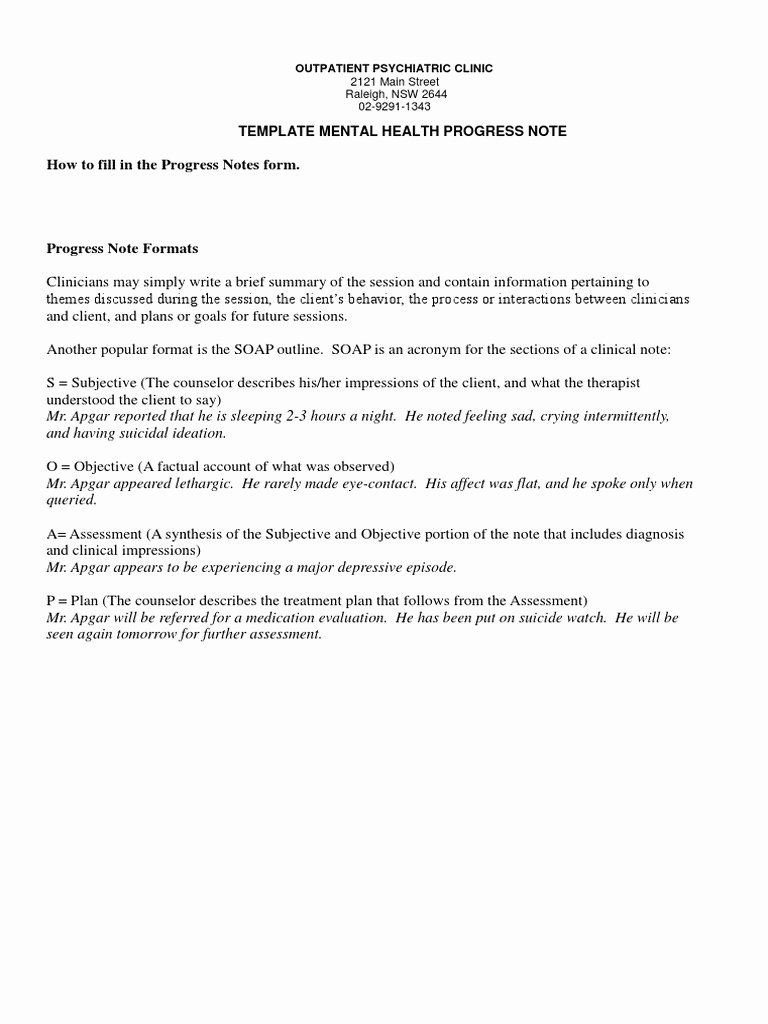
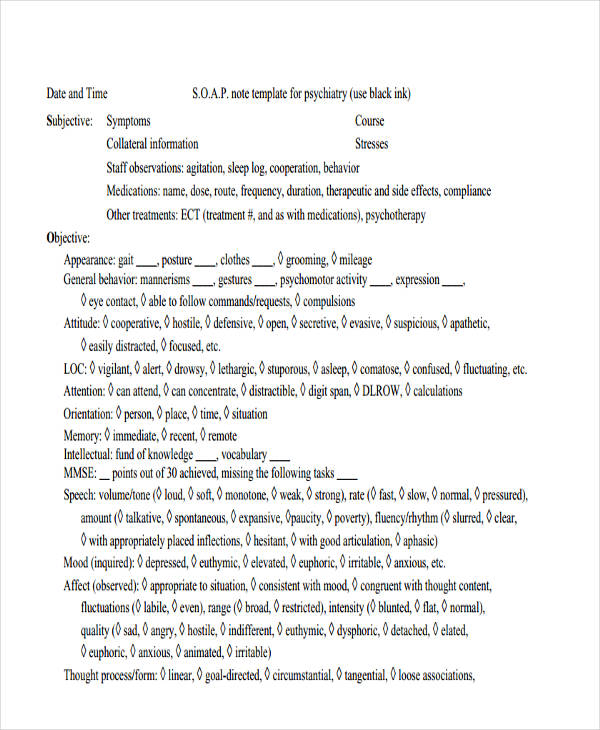
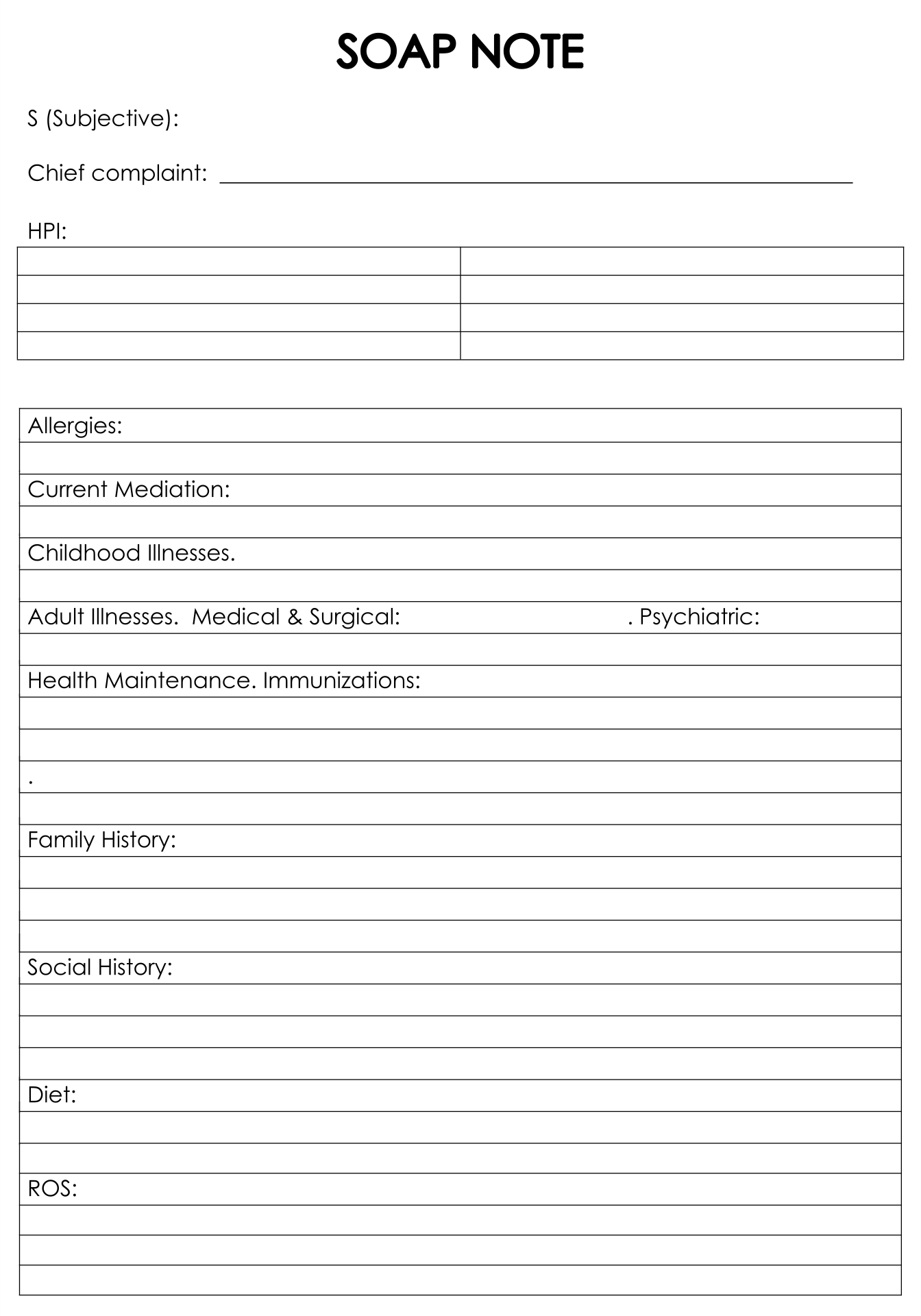
Soap Notes Mental Health Examples. Paper work can be a drag, being better informed about clinical note writing like soap format and having a quality form makes your job easier. Help you gain confidence using soap format; The only words typed by the clinician are highlighted in yellow. Apart from counselling, another area of the medical industry which hugely relies on soap notes is in the treatment of mental health.
 Pin On Counseling Mental Health Soap Note Template Doc IDTcenter From idtcenter.org
Pin On Counseling Mental Health Soap Note Template Doc IDTcenter From idtcenter.org
Consider mental health evaluation referral. Soap notes help a private practice by providing organization, clarity, and a framework for clinical reasoning”. The patient states that what troubles him the. 3+ counseling soap note examples in pdf counseling is an important job to maintain a person’s mental health. At medesk, information about each patient is stored in an individual electronic medical record. This sample so ap note was created using the icanotes behavioral health ehr.
Contact divorce support group and discuss schedule with counselor at next session.
October boyles, lpc 123 main street, suite 202 anywhere, us 1234 5 tel: You probably already know this, but. Consider mental health evaluation referral. Help you gain confidence using soap format; Having an easy to use soap note like our editable pdf soap notes allow practitioners to easily store client and patient notes, organized by each session that they attend. Soap is a very popular format mental health use to document important details from the client’s session.
 Source: klauuuudia.blogspot.com
Source: klauuuudia.blogspot.com
Most mental health clinicians utilize a format known as soap notes. This sample so ap note was created using the icanotes behavioral health ehr. Some stressful situations in life can negatively impact individuals causing them to undergo a life crisis. An effective soap note is a useful reference point in a patient�s health record, helping improve patient satisfaction and quality of care. Example for soap notes for counseling.
![]() Source: icanotes.com
Source: icanotes.com
When health care providers are not using the same framework for notes, it�s easy for critical information to get lost in translation when the next provider accesses the information. At medesk, information about each patient is stored in an individual electronic medical record. Using a template such as soap note means that you can capture, store and interpret your client�s information consistently, over time. Begin to wear a watch and increase awareness of daily schedule. Use words like “discussed” or “talked about” or “reviewed.
 Source: idtcenter.org
Source: idtcenter.org
Writing quality and concise soap notes without skipping the important records is a skill. While mental health soap notes are primarily used to document patient observations, sessions and treatment, soap documentation also helps you progress a patient through the following workflow of practice management: Write your note as if. However, soap notes hold the utmost significance for a mental health professional like you for your client’s future treatment. Soap notes are extremely helpful in counseling.
 Source: pinterest.nz
Source: pinterest.nz
Soap note patient # s: All the notes that you will be taking will determine the quality of care you give to the patients. Israel was approached for ot while in. Soap notes help a private practice by providing organization, clarity, and a framework for clinical reasoning”. Mark and presented by donna wapner.
 Source: bestprofessionaltemplate01.blogspot.com
Source: bestprofessionaltemplate01.blogspot.com
Begin to wear a watch and increase awareness of daily schedule. Example for soap notes for counseling. An effective soap note is a useful reference point in a patient�s health record, helping improve patient satisfaction and quality of care. Soap notes can be used by many different providers across different medical disciplines. However, soap notes hold the utmost significance for a mental health professional like you for your client’s future treatment.
 Source: bestprofessionaltemplate01.blogspot.com
Source: bestprofessionaltemplate01.blogspot.com
Relevant information with appropriate details. An effective soap note is a useful reference point in a patient�s health record, helping improve patient satisfaction and quality of care. October boyles, lpc 123 main street, suite 202 anywhere, us 1234 5 tel: 3+ counseling soap note examples in pdf counseling is an important job to maintain a person’s mental health. Using a template such as soap note means that you can capture, store and interpret your client�s information consistently, over time.
 Source: pinterest.ca
Source: pinterest.ca
Information written in present tense, as appropriate. Use language that is culturally sensitive. Soap notes can be used by many different providers across different medical disciplines. Relevant information with appropriate details. Some stressful situations in life can negatively impact individuals causing them to undergo a life crisis.
 Source: soulcompas.com
Source: soulcompas.com
Paper work can be a drag, being better informed about clinical note writing like soap format and having a quality form makes your job easier. The patient states that what troubles him the. Complete tx plan goal #1, objective 1. This option encourages efficiency, coherence, and care consistency. Soap note patient # s:
Using a template such as soap note means that you can capture, store and interpret your client�s information consistently, over time. Information written in present tense, as appropriate. Write your note as if. Help you gain confidence using soap format; 15 soap note examples and templates (healthcare) soap notes are a helpful method of documentation designed to assist medical professionals in streamlining their client notes.
 Source: rudolfbarshai.com
Source: rudolfbarshai.com
Soap notes help a private practice by providing organization, clarity, and a framework for clinical reasoning”. All the notes that you will be taking will determine the quality of care you give to the patients. Notes that are organized, concise, and reflect the application of professional knowledge. This sample so ap note was created using the icanotes behavioral health ehr. Mark and presented by donna wapner.
![]() Source: bigmarker.com
Source: bigmarker.com
Use words like “discussed” or “talked about” or “reviewed. Relevant information with appropriate details. A distinction between facts, observations, hard data, and opinions. Soap note patient # s: All the notes that you will be taking will determine the quality of care you give to the patients.
 Source: peterainsworth.com
Source: peterainsworth.com
While mental health soap notes are primarily used to document patient observations, sessions and treatment, soap documentation also helps you progress a patient through the following workflow of practice management: It takes time to master the skill of creating comprehensive notes that are easy to use especially for other medical professionals. An effective soap note is a useful reference point in a patient�s health record, helping improve patient satisfaction and quality of care. Most mental health clinicians utilize a format known as soap notes. Israel was approached for ot while in.
 Source: examples.com
Source: examples.com
Soap notes emphasize clarity and concision, which helps get every provider on the same page with minimal confusion. Soap notes emphasize clarity and concision, which helps get every provider on the same page with minimal confusion. Soap notes offer concrete, clear language and avoid the use of. An effective soap note is a useful reference point in a patient�s health record, helping improve patient satisfaction and quality of care. Help you gain confidence using soap format;
 Source: pinterest.com
Source: pinterest.com
Information written in present tense, as appropriate. Patient states he feels lonely and has been trying to manage his depression since november 2019. In order to write a progress note for mental health, there are several. Israel was approached for ot while in. Show concrete examples of subjective and objective data;
 Source: printablee.com
Source: printablee.com
While mental health soap notes are primarily used to document patient observations, sessions and treatment, soap documentation also helps you progress a patient through the following workflow of practice management: Patient states he feels lonely and has been trying to manage his depression since november 2019. Soap notes can be used by many different providers across different medical disciplines. Information written in present tense, as appropriate. Use language common to the field of mental health and family therapy.
 Source: ananicolichphotography.blogspot.com
Source: ananicolichphotography.blogspot.com
Consider mental health evaluation referral. Having an easy to use soap note like our editable pdf soap notes allow practitioners to easily store client and patient notes, organized by each session that they attend. The patient states that what troubles him the. Example for soap notes for counseling. Mental health providers will find soap notes beneficial for creating treatment plan documentation in particular.
![Tips for Writing Better Mental Health SOAP Notes [Updated 2021] Tips for Writing Better Mental Health SOAP Notes [Updated 2021]](https://www.icanotes.com/wp-content/uploads/2018/04/WHAT-ARE-SOAP-NOTES_-min-768x1920.png) Source: icanotes.com
Source: icanotes.com
Soap notes are extremely helpful in counseling. You probably already know this, but. Therapy soap notes follow a distinct structure that allows medical and mental health professionals to organize their progress notes precisely. Soap is an acronym that stands for: Write your note as if.
 Source: pinterest.com.au
Source: pinterest.com.au
This option encourages efficiency, coherence, and care consistency. Writing quality and concise soap notes without skipping the important records is a skill. Digital soap notes can be filled directly into the patient�s medical card during or after the consultation, thanks to the embedded mental health progress note templates. Patient states he feels lonely and has been trying to manage his depression since november 2019. At medesk, information about each patient is stored in an individual electronic medical record.
If you find this site helpful, please support us by sharing this posts to your preference social media accounts like Facebook, Instagram and so on or you can also bookmark this blog page with the title soap notes mental health examples by using Ctrl + D for devices a laptop with a Windows operating system or Command + D for laptops with an Apple operating system. If you use a smartphone, you can also use the drawer menu of the browser you are using. Whether it’s a Windows, Mac, iOS or Android operating system, you will still be able to bookmark this website.
Category
Related By Category
- Metastatic thyroid cancer prognosis
- Endocrinologist diabetes type 2
- How fast does colon cancer spread
- Hip replacement in elderly
- Physical therapy after arthroscopic shoulder surgery
- Symptoms of bacterial meningitis in children
- Chromophobe renal cell carcinoma
- Eye color change surgery usa
- Pradaxa vs eliquis vs xarelto
- Advanced stomach cancer symptoms